Abstract
Introduction
T-Large Cell Granular Lymphocytic Leukemia (T-LGLL) is a rare lymphoproliferative disorder with an incidence of 2-3% of all mature lymphoid leukemias. Progressive/symptomatic T-LGLL which mainly presents with cytopenia's is very rare compared to the indolent forms. Given the rarity of the disease, limited literature is available about the epidemiology, survival, and development of secondary primary malignancies (SPMs) in T-LGLL.
Methodology
We used the November 2020 submission of the Surveillance, Epidemiology and End Results (SEER) 17 registry, which covers ~27.8% of the US population based on the 2010 census to identify all cases of T-LGL diagnosed between 2000-2019. We identified all cases using the International Classification of Diseases for Oncology edition 3 (ICD-O-3) code. Kaplan Meir method is used for survival analysis and standardized incidence ratio (SIR) or relative risk and absolute excess risk (AER) were calculated for SPM. This retrospective analysis was performed using SEER*Stat version 8.3.6 statistical software and STATA.
Results
A total of 2,297 cases were identified during the study period. The age-adjusted incidence rate of T-LGLL in the United States was 0.2 cases per 100,000 individuals. The incidence rate was higher in elderly patients (age >= 65 years) highest incidence was observed in 80-84 years. The median age of diagnosis was 66 years. Males were 52% (n= 1209) and females were 48% (n= 1093). Predominant race was Caucasians (81%) followed by Blacks 9.4%. The overall survival (OS) of the entire cohort at 1 year (yr), 3 yr, 5 yr was 92%, 84.8% and 80%. 5-yr OS was 77.2% in males and 82.6% in females. Caucasians had a 5-y OS of 78% and blacks had 88%.
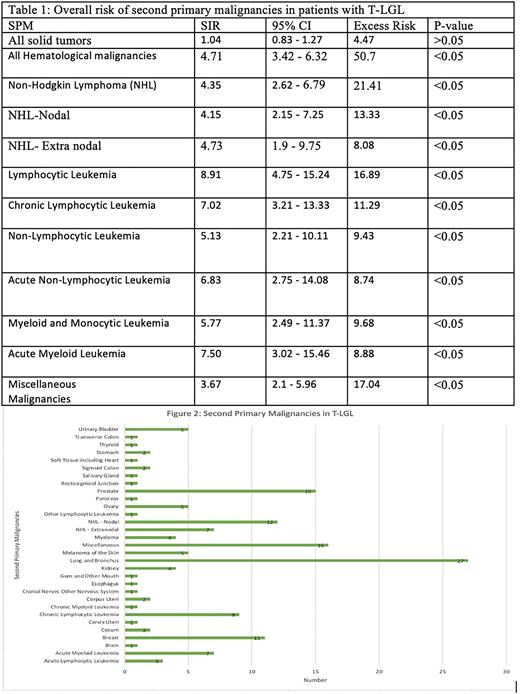
For SIR analysis, 1668 patients with T-LGLL as the primary malignancy were included. 139 (8.3%) patients developed SPM with a total of 151 SPMs. The median latency period for the development of SPMs was 25.5 (range= 5-209) months. T-LGLL patients had an overall increased risk of developing SPM than the general population (SIR= 1.48, 95% CI= 1.25-1.75, AER= 71.45, p< 0.05). Regarding solid tumors, this was predominantly observed in ovarian malignancy (SIR= 4.8, 95% CI= 1.5-10.7, AER= 5.72, p<0.05) followed by lung and bronchus (SIR= 1.88, 95% CI= 1.24- 2.74, AER= 18.55, p<0.05). Secondary hematological malignancies were predominantly lymphoma (SIR= 4.14, 95% CI = 2.5-6.5, AER= 21.09, p<0.05) and leukemia (SIR= 7, 95% CI= 4.3- 10.6, AER = 26.3, p<0.05) with acute lymphocytic leukemia (ALL) being the highest observed SPM (SIR= 31.3, 95% CI= 6.5- 91.5, AER = 4.25, p<0.05) (rest in table 1). The rate of overall SPM in T-LGLL after 1 yr (SIR= 8.2, 95% CI= 4.5-13.8, AER=98), 1- 5 yrs (SIR= 4.67, 95% CI= 2.99-6.94, AER= 49.92) and 10+ yrs (SIR= 2.84, 95% CI = 1.04-6.2, AER= 25.2) from diagnosis of T-LGLL was significantly higher than in the general population (all p<.05). This trend was not observed in the interval 5-10 yrs after diagnosis. Among T-LGLL patients, the risk of developing ALL was significantly higher within 1-yr after the diagnosis (SIR= 144.7, 95% CI= 13.9-414.2, ER= 15.8, p<0.05). The risk of development of solid tumor malignancies was significantly higher than the rest of the population only 10 yrs after the diagnosis of T-LGLL (SIR= 3.11, 95% CI = 1.6-5.77, AER= 285.11, p<0.05). Overall, tumors of lung and bronchus (17%), miscellaneous malignancies (10.6%), prostate (9.9%) were the most observed SPMs (Figure 1).
Conclusion
To our knowledge, this is the first comprehensive study assessing the incidence of SPMs in T-LGLL from a national database. The risk of SPM is higher in patients with T-LGLL compared to the general population especially 1 yr, 1- 5 yr, 10+ yrs from the diagnosis. The risk of secondary hematological malignancies, predominantly ALL and lymphoma is higher until 10 years from the diagnosis and the overall risk of secondary solid tumor malignancies are higher after 10 years from the diagnosis. T-LGLL patients also have a higher risk of developing lung, ovarian carcinoma compared to the general population. Our studies may help guide survivorship as close follow is needed for T-LGLL patients even after 5 and 10 years of diagnosis. Future studies are warranted to understand the reason for the increased development of SPM in T-LGLL patients and to specify the subtypes of secondary lymphoma's and ALL to understand the transformation pattern of T-LGL.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal